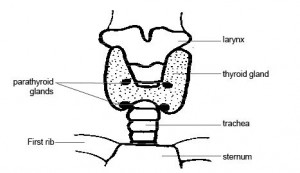
The parathyroid glands are four pea-sized glands in the neck. They are normally found in pairs on each side of the neck adjacent to the thyroid gland. Their function is unrelated to the thyroid gland and they share the name only because of their location; ‘para’ is derived from the Greek for ‘beside’: para(beside)thyroid.
 The parathyroids excrete a hormone called parathyroid hormone (PTH), which controls calcium levels in the body. Calcium is stored in the bones and released into the bloodstream to help with muscle contraction and nerve stimulation. The parathyroid glands monitor and regulate calcium levels in the blood by releasing PTH when calcium levels get too low. PTH raises the blood calcium level by stimulating bone to release calcium and the intestine to absorb more calcium from food.
The parathyroids excrete a hormone called parathyroid hormone (PTH), which controls calcium levels in the body. Calcium is stored in the bones and released into the bloodstream to help with muscle contraction and nerve stimulation. The parathyroid glands monitor and regulate calcium levels in the blood by releasing PTH when calcium levels get too low. PTH raises the blood calcium level by stimulating bone to release calcium and the intestine to absorb more calcium from food.
Indications for surgery
Primary hyperparathyroidism is the most common indication for removal of parathyroid glands. This condition is due to excessive PTH production from one or more overactive parathyroid glands. The affected hyperactive gland/s don’t recognise that blood calcium levels are high enough and continue to release PTH. This may lead to symptoms including osteoporosis, kidney stones, irritability, bone pain, poor sleeping pattern and fatigue. Normal parathyroid glands tend to stop their production of PTH and lie dormant while the affected parathyroid/s continue to release excessive amounts of PTH. Removal of the affected parathyroid/s results in a rapid return to normal blood calcium levels with many patients noting a marked improvement in symptoms such as bone pain, sleep pattern, mood and energy levels.
Surgical treatment
Minimally-invasive parathyroidectomy
Modern surgical techniques use a focussed ‘minimally-invasive’ key-hole approach to target the affected parathyroid glands. The surgeon uses preoperative imaging to localise the gland and remove it through a tiny incision of about 2cm placed in a skin crease of the neck. Sutures are used to close the wound is closed with a technique called “continuous subcuticular suture” which particularly enhances the cosmetic result. Drains are not used. Patients are admitted to hospital on the day of surgery and usually discharged the morning after.
Minimally-invasive video-assisted parathyroidectomy
Minimally-invasive video-assisted parathyroidectomy uses the key-hole approach described above with the addition of a high-definition camera to assist the surgeon to visualise the parathyroid gland/s, nerves and surrounding structures.
The neck of a young patient 4 weeks after minimally invasive neck surgery
PICTURE